Abstract
Somatic mutations in isocitrate dehydrogenase (IDH) genes are seen in ~20% of adult patients with acute AML, with hotspot mutations in IDH2 (R172, R140) being more common (15%) compared to IDH1 (R132; 5-7%). We previously reported a higher 1-year relapse rate after allogeneic hematopoietic cell transplantation (alloHCT) in AML patients harboring IDH mutations compared to those without IDH mutations. (Salhotra el, Clin Lymphoma Myeloma Leuk. 2019). Similar results were observed by Chen et al in a larger multicenter retrospective study. Enasidenib is a selective inhibitor of mutant IDH2 (mIDH2) enzymes, which has shown single agent activity in patients with relapsed/refractory AML with overall response rate of 40% and a median response duration of 5.8 months. We hypothesized that Enasidenib as post-HCT maintenance therapy is safe, well-tolerated and can improve survival outcomes in AML patients carrying mIDH2. Here, we are reporting results of our multicenter [City of Hope (COH) and Moffitt Cancer Center (MCC)] pilot trial of Enasidenib as maintenance after alloHCT in IDH2 mutated AML patients (NCT03728335).
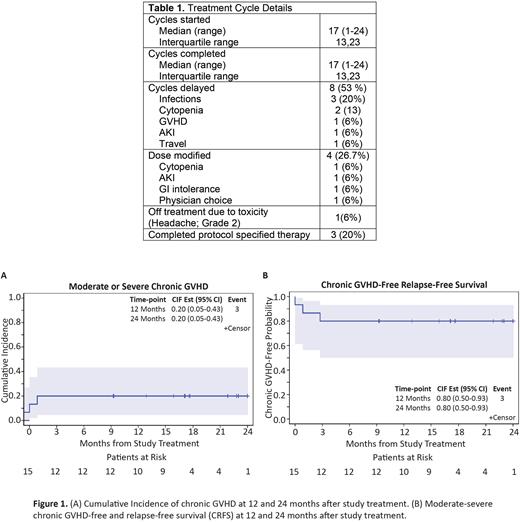
Recipients of alloHCT who had AML (n=15) with IDH2 mutations at the time of diagnosis were prospectively enrolled in this trial. Patients were eligible for maintenance therapy irrespective of conditioning regimen, if in complete remission (CR) at day +30 post-HCT, had ECOG PS ≤2 and adequate marrow function defined as ANC ≥1000/µL; Hemoglobin ≥10gm/dL and platelets ≥ 50,000/µL. Patients with grade ≥2 acute graft-versus-host disease (GVHD) were excluded. Enasidenib was given at the FDA approved dose of 100 mg/day between days 50 and 120 post-HCT for 2 years in 28 days cycles. The primary objective was to evaluate safety and tolerability of enasidenib as post-HCT maintenance therapy. Toxicities were scored by the NCI-CTCAE v5.0. Secondary objectives were to assess overall survival (OS), leukemia-free survival (LFS), non-relapse mortality (NRM), relapse, and 1-year chronic GVHD-free and relapse-free survival (CRFS). Sample size of 15 was determined based on modified rule of continuous monitoring for toxicity using Pocock-boundary with desired probability of early stopping of 0.75 if the unacceptable toxicity rate was ≥33%.
From August 2020 to July 2021, we enrolled 15 patients (8 at COH and 7 at MCC) who were eligible after day +30 bone marrow biopsy documented remission. The median age was 58 years (range: 24-77); Male: Female ratio was 40:60% and 67% of patients were Caucasian. Pre-transplant remission status was CR1 in 73% (n=7), CR2 in 20% (n=3) and measurable residual disease positive in 6% (n=1). Cytogenetic risk classification was intermediate in 60% (n=9), adverse in 26% (n=4), and favorable risk in 13% (n=2) of patients. Median time to start maintenance post HCT was 104 days (range: 54-119). Donors were 8/8 HLA matched unrelated (53%; n=8), HLA identical related (20%; n=3), or haploidentical (26%; n=4). Most patients (80%; n=12) received reduced intensity conditioning, and mobilized peripheral blood was the graft source used in all study patients. GVHD prophylaxis consisted of post-transplant cyclophosphamide-based (60%; n=9) or tacrolimus-based (40%; n=6) regimens (Tac/Siro= 4 and Tac/MTX= 2).
At the data cutoff of June 2022, enrolled patients completed a median of 17 cycles (range: 1-24) of enasidenib maintenance. We collected all grades of adverse effects (AEs) during the first 2 cycles, and grade ≥3 AEs for subsequent cycles. In the first 2 cycles, grade ≥3 AEs were mainly due to hematologic toxicity including: lymphopenia (26%; n=4), anemia (20%; n=3), neutropenia (13%; n=2), and thrombocytopenia (6%; n=1). Non-hematologic AEs were grade 1-2 nausea (60%; n=9), and vomiting/diarrhea (26%; n=4). Table 1 shows the summary of treatment cycles. At median follow up of 17.1 months (range: 7.0-25.9) the 1 and 2-year OS and LFS probabilities were 100%. The cumulative incidence of moderate to severe chronic GVHD at 1-year was 20% and 1-year CRFS was 80% (Figure 1).
In conclusion, post-HCT enasidenib maintenance therapy was safe and well-tolerated, resulting in favorable survival outcomes in AML patients carrying IDH2 mutations. While treatment delays and dose reductions were common, the majority of the study patients remained on the protocol therapy. Droplet digital PCR testing on bone marrow was done to study clearance of IDH2 clones post-HCT and these results will be available by December 2022.
Disclosures
Salhotra:BMS: Research Funding; Kadmon: Other: Advisory board meeting ; Orca Bio: Research Funding. Bejanyan:Medexus Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees; Magenta Therapeutics: Consultancy, Membership on an entity's Board of Directors or advisory committees; CareDX Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees; Sanofi: Consultancy, Membership on an entity's Board of Directors or advisory committees; CTI BioPharma: Consultancy, Membership on an entity's Board of Directors or advisory committees. Al Malki:CareDx: Consultancy, Research Funding; NexImmune: Consultancy, Research Funding; Gilead: Consultancy, Research Funding; Incyte: Consultancy, Research Funding; Miltenyi Biotec: Consultancy, Research Funding; Hasna Biopharma: Membership on an entity's Board of Directors or advisory committees. Faramand:Kite/Gilead: Research Funding; Novartis: Research Funding. Aldoss:Jazz Pharmaceuticals: Honoraria, Speakers Bureau; Autolus Limited: Consultancy; Amgen: Consultancy; Agios: Consultancy, Honoraria; AbbVie: Consultancy, Research Funding; Kite: Consultancy. Artz:Abbvie: Honoraria; Magenta: Honoraria. Aribi:SeaGen: Consultancy. Ball:Oncovalent: Membership on an entity's Board of Directors or advisory committees. Pullarkat:AbbVie, Amgen, Genentech, Jazz Pharmaceuticals, Novartis, Pfizer, and Servier: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen, Dova, and Novartis: Consultancy, Other: Advisory Board Member. Marcucci:Novartis: Other: Speaker and advisory scientific board meetings; Agios: Other: Speaker and advisory scientific board meetings; Abbvie: Other: Speaker and advisory scientific board meetings. Nakamura:BluebirdBio: Consultancy; Omeros: Consultancy; Sanofi: Consultancy; Helocyte Inc: Research Funding; Magenta Therapeutics: Consultancy; Kadmon: Consultancy. Stein:Amgen: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal